SAFER SIX
TorontoA sex-positive, body-positive, pro-choice, and inclusive health clinic offering comprehensive STBBI prevention, testing, and treatment services.
Visit website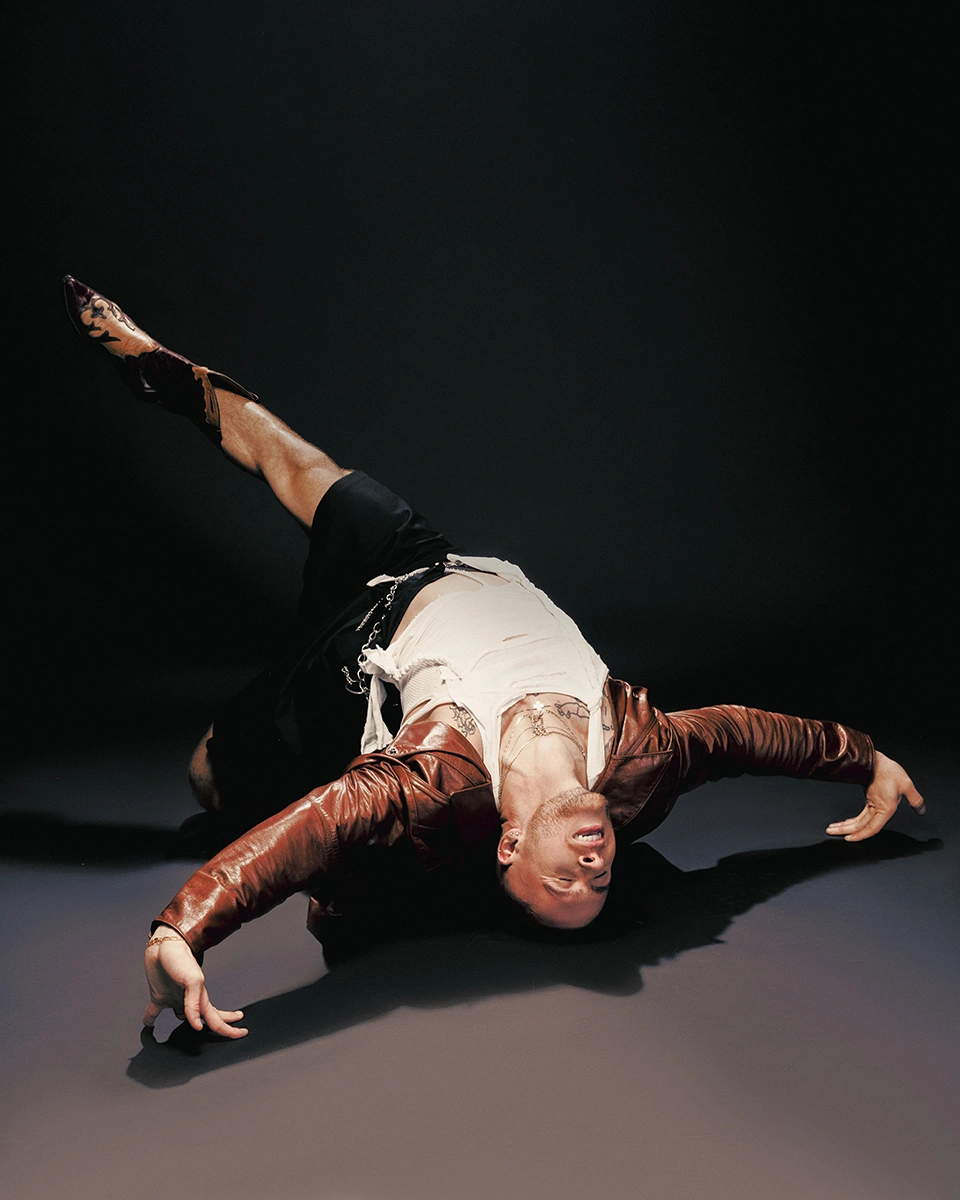


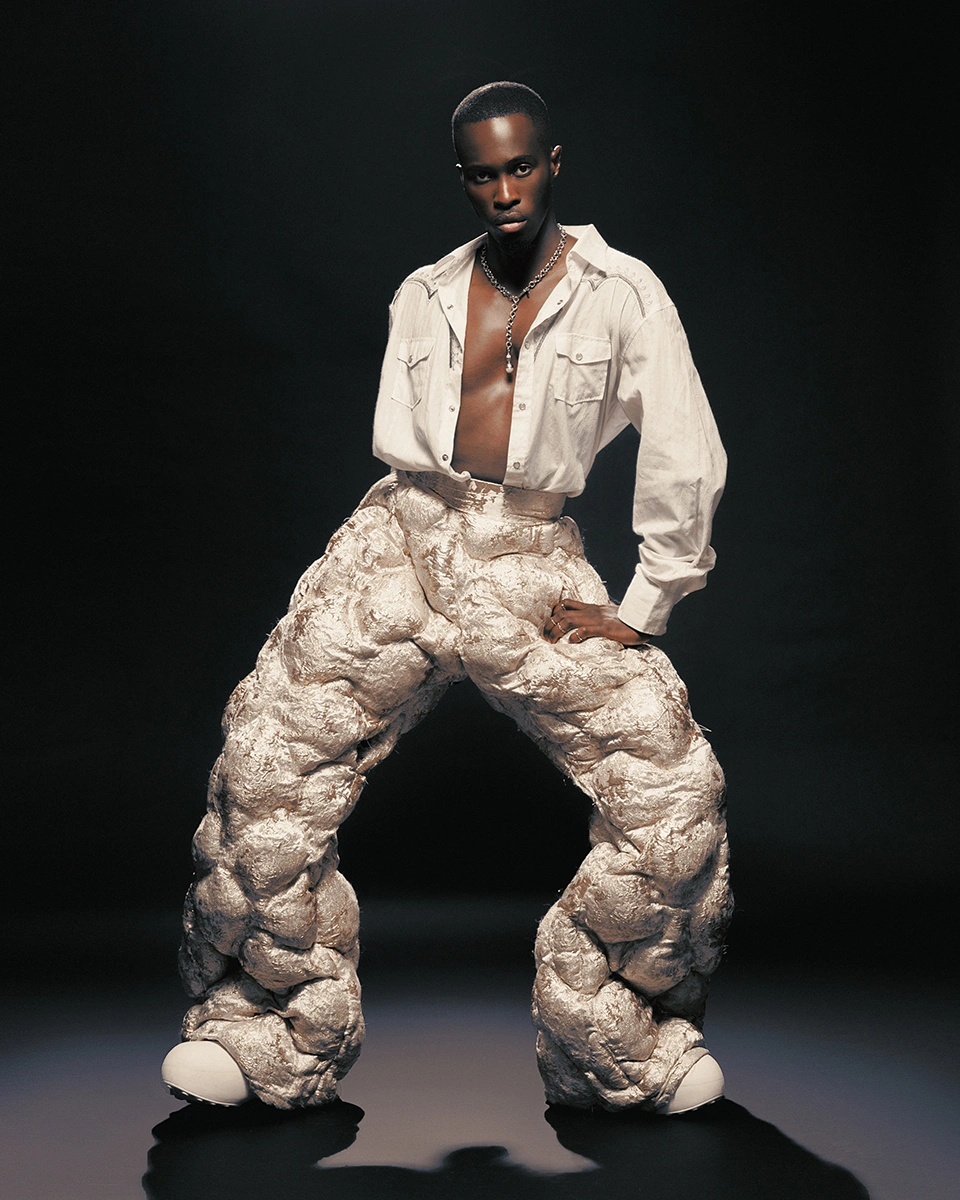
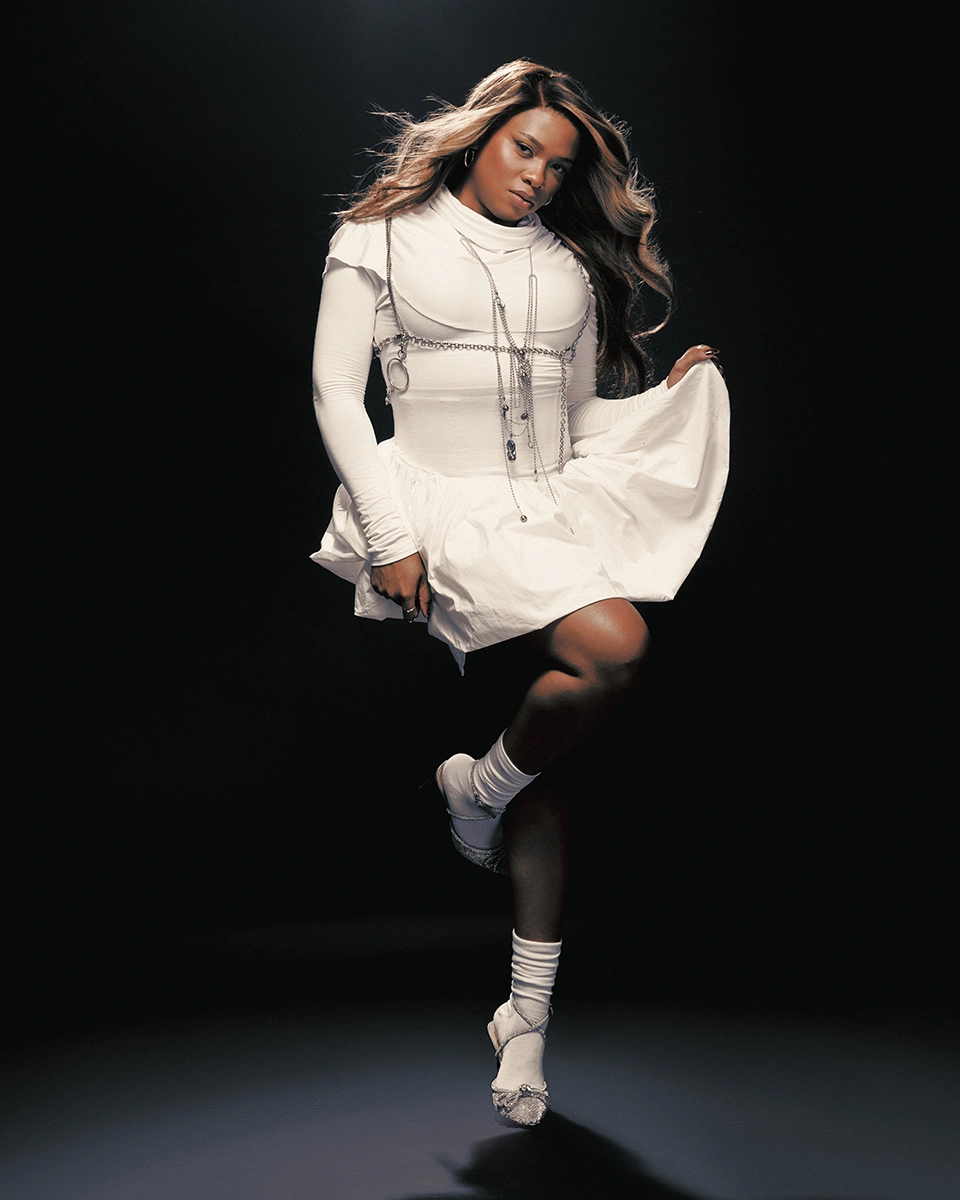


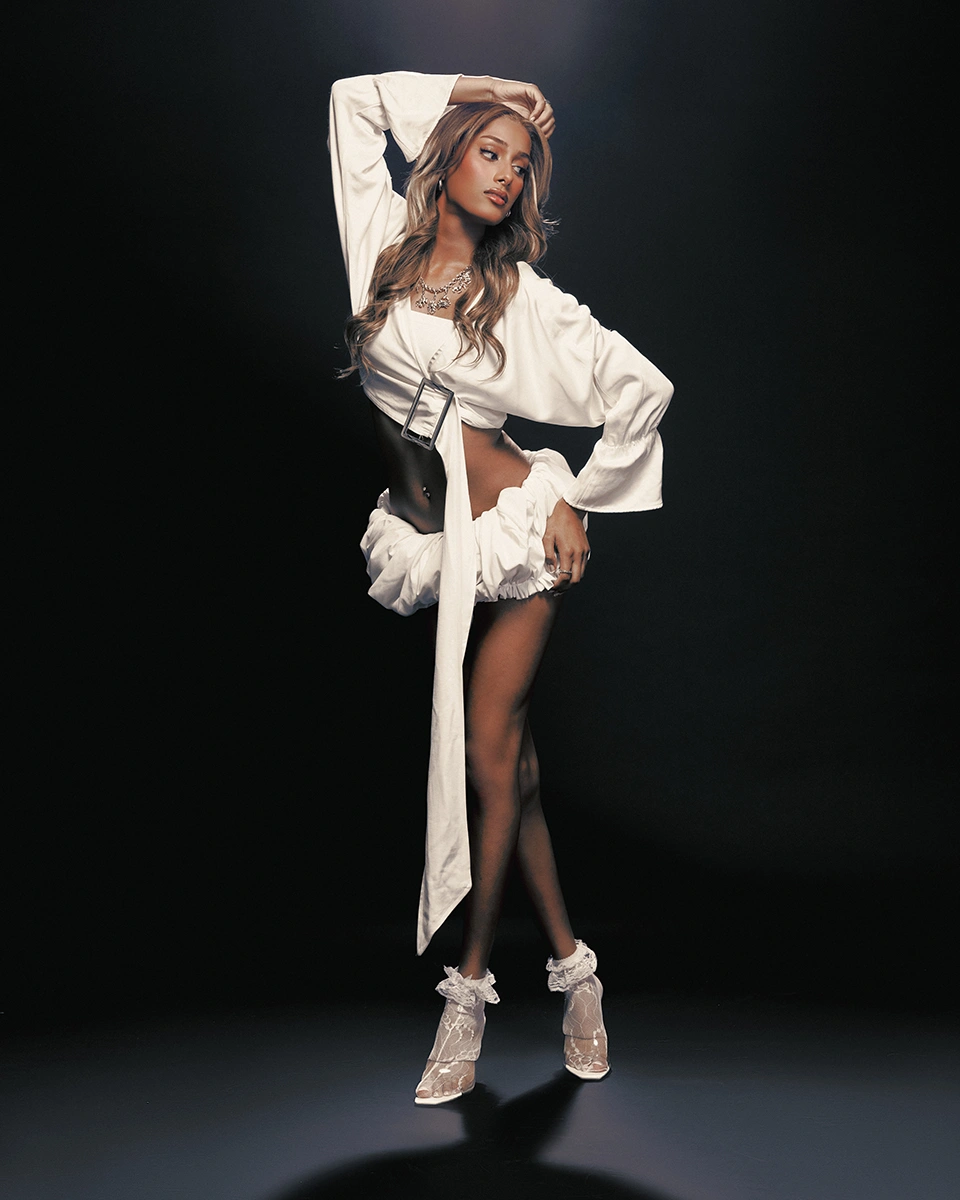
We've always needed each other—chosen family and community helping mend the parts of ourselves that get scuffed on the journey to self-acceptance. This is no different. Stigma has held us back for far too long, casting our loved ones living with HIV aside. Through the power we share in unity, let's build a future where we all feel seen, safe, and worthy of love.
Experience the crown jewel of Canadian Ballroom. Join us this December 7th at HISTORY for an unforgettable night.
Your wallet or glove compartment? Not the spot. Heat and friction can weaken latex and put you at risk.
Condoms expire, and old ones leave you at greater risk of contracting sexually transmitted infections or getting pregnant.
Teeth and sharp objects are a no-go. Tiny tears can compromise a condom's integrity and overall effectiveness.
Without enough space in the reservoir, fluids could spread along the condom and overflow, risking exposure to your partner.
Halfway is risky business. Full coverage is the only way to ensure maximum safety.
Keep it tight and secure. Ensuring everything stays in place means no spills, no mess, and no surprises.
Reusing an old condom puts you at risk. Start fresh every single time to keep you and your partner safe.
Two is not better than one—it causes friction and increases the risk of breakage.
Oil-based lubricants? Absolutely not. They weaken latex and can cause it to tear.
While natural condoms protect against pregnancy, they're not recommended for the prevention of STIs.
PrEP is for ongoing prevention before potential exposure, while PEP is for emergencies after potential exposure.
Adherence to PrEP is crucial. If not taken as prescribed, there may not be enough medication in the body to reduce the risk of HIV infection.
It takes at least 7 days for PrEP to offer maximum protection for anal sex and about 20 days for frontal sex.
PrEP is highly effective, and pairing it with other safer sex practices—like using condoms and getting tested regularly—offers even greater protection.
Gaps in PrEP coverage mean you’ll need to start fresh. An HIV test ensures you’re protected right from the beginning.
Timing is critical—PEP should be started within 72 hours of potential exposure to be effective. The sooner, the better.
No cutting corners. For PEP to work effectively, you must complete the full 28-day treatment without missing any doses.
PEP is intended for emergency situations and shouldn't replace regular prevention methods like PrEP and condom use.
Both PrEP and PEP can have side effects, such as nausea or headaches. Discuss any concerns with your healthcare provider.
Regular check-ins with your doctor help monitor your health and ensure PrEP or PEP is working as intended.
HIV targets the immune system, weakening the body’s ability to fight infections. Viral load refers to the amount of HIV present in the blood.
Effective antiretroviral therapy lowers your viral load to undetectable levels. In Canada, this usually means below 40 or 50 copies per milliliter of blood.
An undetectable viral load means that the virus levels in your blood and sexual fluids are so low that you cannot pass on HIV to sexual partners.
Reaching and maintaining an undetectable viral load generally requires about six months of consistent antiretroviral therapy.
Get tested regularly. Early diagnosis and early initiation of treatment can help you reach undetectable status sooner.
U=U is a powerful tool in a broader arsenal that includes education, safer sex practices, regular screenings, and other prevention methods.
Providing universal access to ART empowers more individuals to reach and maintain undetectable status, benefiting both personal and public health.
Start with your circle. Promoting U=U encourages open conversations, helps dismantle stigma, and fosters a deeper understanding of HIV.
U=U is backed by decades of research and real-world evidence, proving that effective treatment stops sexual transmission entirely.
While U=U prevents HIV transmission, condoms remain key for comprehensive STI prevention.
It takes all of us—and we need you. Join us in building a future that's inclusive, compassionate, and free of HIV stigma.
1,536
pledges
and counting
A sex-positive, body-positive, pro-choice, and inclusive health clinic offering comprehensive STBBI prevention, testing, and treatment services.
Visit websiteA community-focused healthcare centre for cisgender men who are into men, as well as two-spirit, transgender, and non-binary individuals, providing rapid STBBI testing and holistic health and wellness services.
Visit websiteA pioneering organization dedicated to reducing new HIV infections and providing life-affirming care for individuals living with HIV/AIDS.
Visit websiteA clinic focused on HIV and STBBI prevention for gay, bisexual, queer men, and trans and gender-diverse individuals, offering inclusive and accessible services.
Visit websiteA welcoming space for gay, bisexual, queer men, and trans and gender-diverse individuals, offering free routine testing, sexual health education, and comprehensive programs and services.
Visit websiteA community-based organization, providing evidence-informed, non-judgmental sexual health programs and services, including STBBI testing.
Visit websiteA national grassroots initiative providing free HIV self-testing kits and support to empower individuals and reduce stigma.
Visit websiteA trusted hub for the latest HIV information and a directory connecting people across Canada to HIV, hepatitis C, sexual health, and harm reduction services.
Visit websiteA comprehensive online resource offering accurate and up-to-date information about HIV prevention, testing, treatment, and long-term care.
Visit website